Click here to purchase ASSURE-100 on Amazon.com, or for local Hawaii pick-up, click here to purchase from our Shopify site.
The Impact of SARS-CoV-2 on Blood Vessels
Direct and Indirect Damage
SARS-CoV-2 primarily enters cells via the ACE2 receptor, which is abundantly expressed in endothelial cells lining blood vessels. This interaction can lead to:
- Endothelial Dysfunction: The virus directly damages endothelial cells, impairing their ability to regulate blood flow and prevent clot formation.
- Inflammatory Response: COVID-19 triggers a systemic inflammatory response, exacerbating vascular damage and increasing the risk of thrombosis (blood clots).
Microvascular Complications
Research indicates that SARS-CoV-2 can harm small blood vessels, resulting in:
- Capillary Leakage: Damage to tiny blood vessels can lead to fluid leakage, contributing to tissue swelling and organ dysfunction.
- Microthrombi Formation: Small clots can form in the capillaries, disrupting oxygen delivery to vital organs.
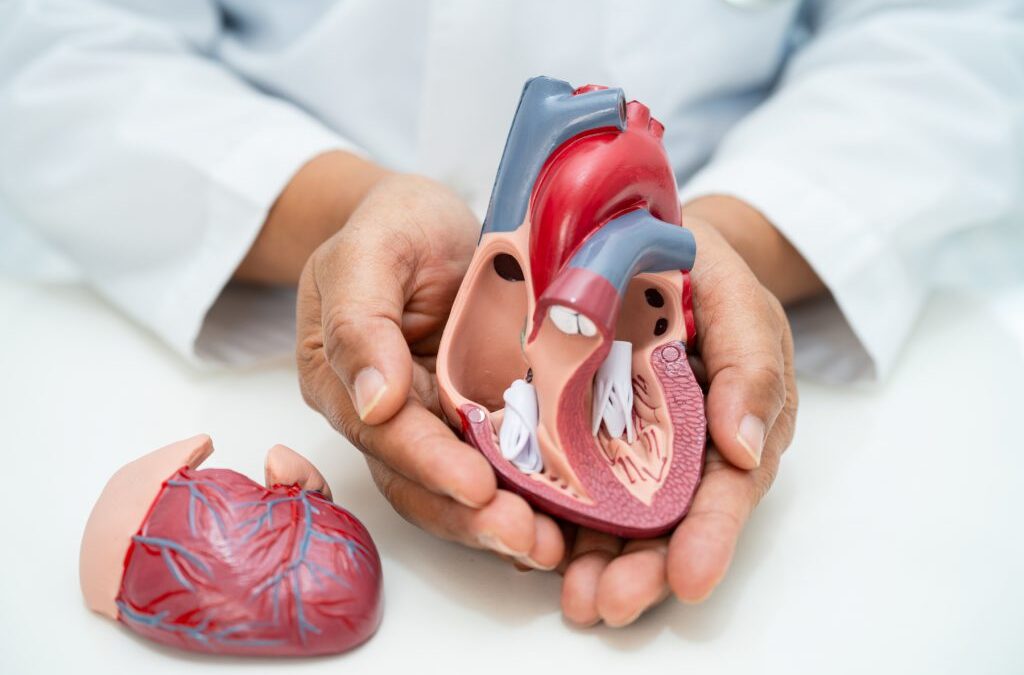
COVID-19’s Effects on Heart Health
Myocardial Injury
Heart muscle damage, or myocardial injury, is a common complication in severe COVID-19 cases. It can occur due to:
- Direct Viral Invasion: SARS-CoV-2 may directly infect heart cells.
- Inflammation: The systemic inflammatory response can inflame the heart (myocarditis), impairing its ability to pump blood effectively.
- Oxygen Deprivation: Severe cases often involve hypoxia, straining the heart.
Arrhythmias and Heart Failure
Patients with COVID-19 are at increased risk of arrhythmias (irregular heartbeats) and heart failure, particularly those with preexisting cardiovascular conditions. These complications are driven by:
- Electrolyte Imbalances: Infections can disrupt electrolytes essential for maintaining a steady heartbeat.
- Increased Cardiac Workload: The heart compensates for systemic inflammation and oxygen deprivation by working harder, potentially leading to failure.
Long COVID and Cardiovascular Risks
Long COVID, characterized by persistent symptoms weeks or months after initial infection, has significant implications for cardiovascular health. Common symptoms include:
- Chest Pain: Indicative of ongoing inflammation or vascular dysfunction.
- Palpitations: Resulting from arrhythmias or autonomic nervous system dysregulation.
- Exercise Intolerance: Due to reduced cardiac output or lingering inflammation.
The Role of Rapid Testing in Prevention
Identifying infections early with tools like rapid home tests is crucial for reducing the risk of severe outcomes, including cardiovascular complications. Testing can:
- Help individuals isolate promptly, reducing virus spread and exposure risks for vulnerable populations.
- Facilitate early medical intervention, especially for those with preexisting cardiovascular conditions.
- Provide clarity for post-COVID-19 care plans by confirming infection status.
Who Is Most at Risk?
Certain populations are more vulnerable to the cardiovascular effects of COVID-19:
- Individuals with Preexisting Conditions: Diabetes, hypertension, and prior heart disease increase risk.
- Older Adults: Aging vessels are more susceptible to damage and inflammation.
- Unvaccinated Individuals: Vaccination significantly reduces severe outcomes.
Protecting Your Cardiovascular Health
Vaccination and Boosters
Staying up to date with COVID-19 vaccinations is one of the most effective ways to prevent severe illness and its cardiovascular complications. Vaccines reduce viral load and inflammation, protecting both the respiratory and cardiovascular systems.
Regular Monitoring
Those with a history of cardiovascular conditions should:
- Monitor for symptoms such as chest pain, shortness of breath, and palpitations.
- Use rapid home tests at the first sign of illness to confirm infection and seek timely care.
Lifestyle Adjustments
Adopting heart-healthy habits can mitigate risks:
- Diet: Emphasize fruits, vegetables, and lean proteins.
- Exercise: Engage in regular, moderate physical activity.
- Stress Management: Practice relaxation techniques to reduce inflammation-inducing stress.
Future Research and Treatments
The scientific community continues to study the long-term cardiovascular effects of COVID-19. Areas of focus include:
- Developing targeted therapies to repair endothelial damage.
- Identifying biomarkers for early detection of cardiovascular complications.
- Exploring rehabilitation programs for long COVID patients with persistent heart symptoms.
COVID-19’s impact on blood vessels and the heart underscores the virus’s complexity and far-reaching effects. By staying informed, using preventive tools like rapid home tests, and adopting proactive health measures, individuals can protect their cardiovascular health. As research advances, the integration of these insights into clinical care will be crucial for reducing the pandemic’s long-term toll on public health.
Click here to purchase ASSURE-100 on Amazon.com, or for local Hawaii pick-up, click here to purchase from our Shopify site.
- Keywords: COVID-19, heart health, blood vessels, SARS-CoV-2, cardiovascular risks, rapid testing, rapid home tests, pandemic heart effects, long COVID
January 22, 2025
Oceanit